- Posterior Capsule Opacification (PCO)
- Eye Stroke (Retinal Artery Occlusions & Retinal Vein Occlusions)
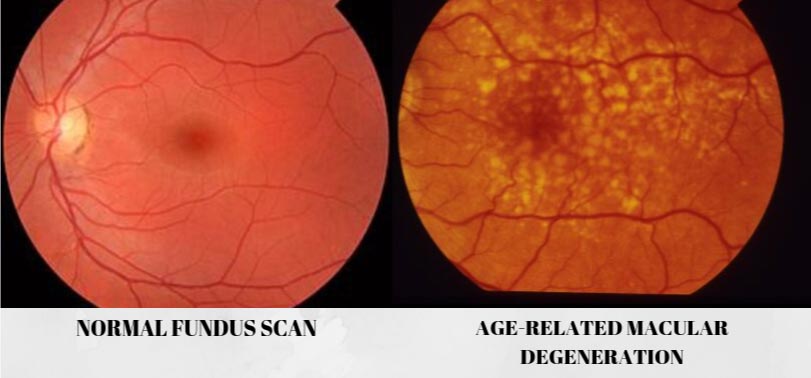
- Age-Related Macular Degeneration (ARMD)
- Macular Hole
- Central Serous Retinopathy (CSR)
- Macular Oedema
- Vitreous Haemorrhage
- Retinal Detachment
- Ocular Hypertension (OHT) & Glaucoma
- Retinitis Pigmentosa (RP)
- Floaters



Posterior Capsule Opacification (PCO)
During cataract surgery, the cloudy lens will be removed, and a synthetic intraocular lens will be implanted inside your eye. However, in some cases, the capsule or the bag that ‘holds’ the artificial lens may become thickened and opaque a few months after the surgery. This condition is called posterior capsule opacification (PCO). As a result, the patient may experience hazy or blurry vision.
Signs and Symptoms
- Blurred and misty vision
- Sensitivity and glare towards light
Who will usually have this?
The likelihood of developing PCO after your cataract surgery depends on the patient’s age, the diabetic status, hardness of the cataractous lens and type of lens implanted. PCO can occur a few months or even years after the surgery.
Treatment/ Management
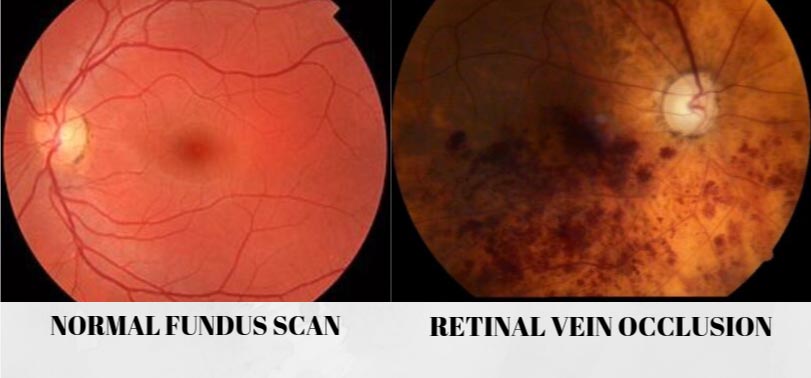
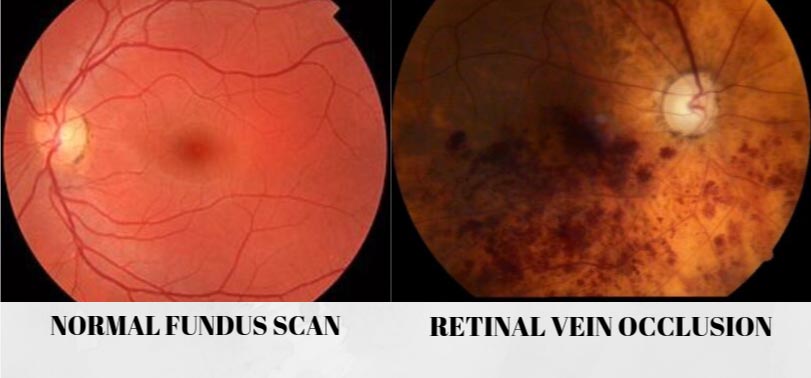
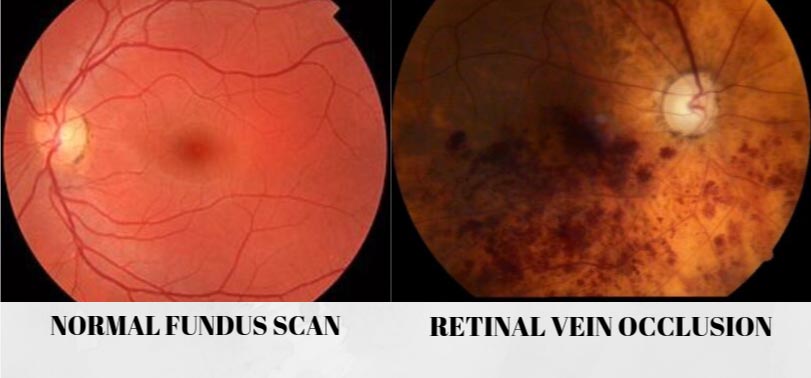
Eye Stroke (Retinal Artery Occlusions & Retinal Vein Occlusions)
Blood vessels in our body consist of both arteries and veins that carry bloods throughout our body, including our precious eyes. However, blockage in the blood vessels leads to impaired nutrition and oxygen supply to the organs. In the eye, it results in vision loss. Retinal artery occlusion occurs when retinal artery is blocked and retinal vein occlusions is when the retinal vein is occluded.
Signs and Symptoms
- Sudden vision loss or blurry vision
- Floaters
Risk Factors
- Ageing
- Hypertension
- Heart problems
- High cholesterol
- Atherosclerosis
- Diabetes mellitus
- Glaucoma
- Smoking
- Obesity
Treatment/Management
- Anti-VEGF injection
- Hyperventilation / hypercapnic breathing
- Lowering intraocular pressure – to loosen the blockage
- Ocular massage
- Eye injection of corticosteroid drugs
- Retinal laser therapy
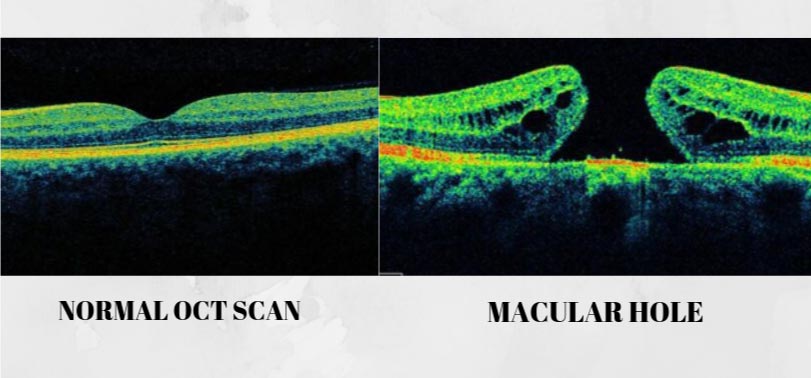
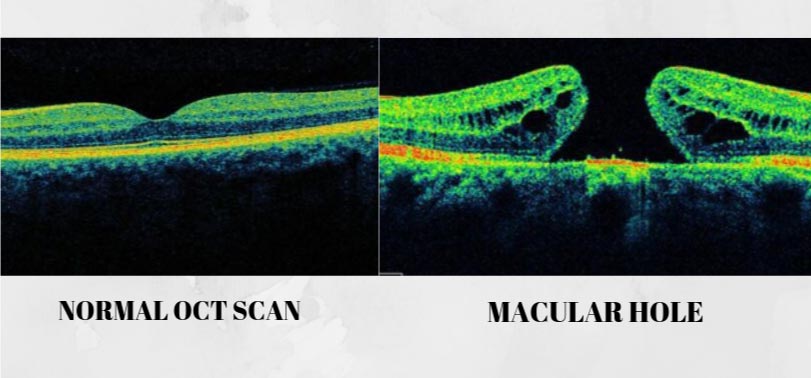
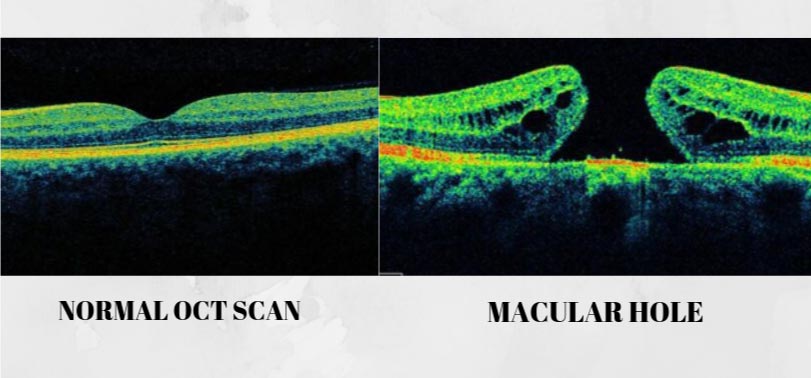
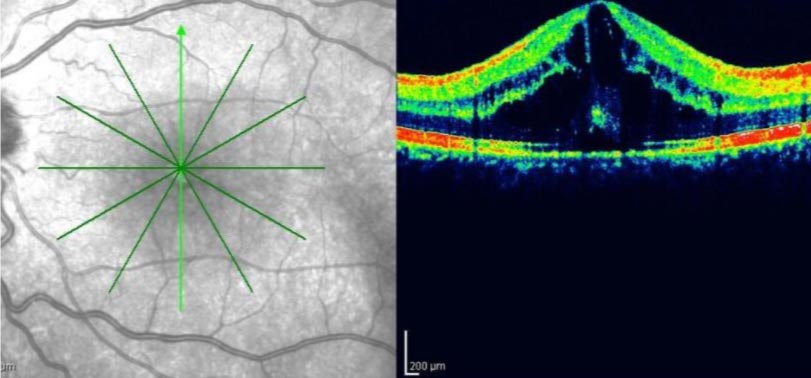
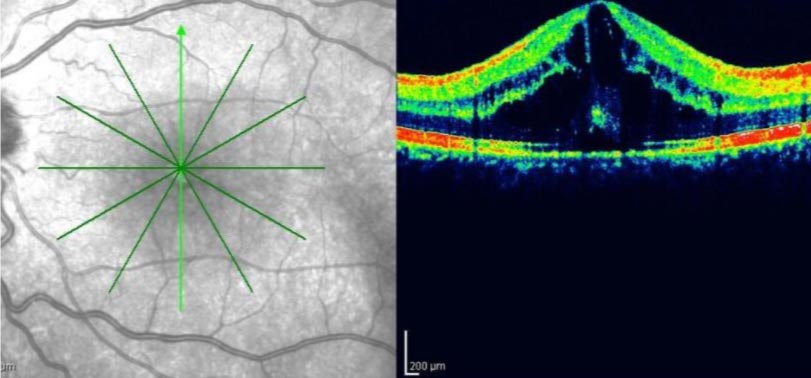
Macular Hole
It is an eye condition where there is a break on the centre portion of the retina called the macula. Macula is vital and responsible for us to focus on our central vision while reading, driving, looking at fine details and recognising faces. Full thickness macular hole (FTMH) affects approximately 3 in 1000 individuals, in the sixth or seventh decade of their life.
Signs and Symptoms
- Severe impairment or dark spot on central vision
- Blurred and distorted central vision (metamorphopsia)
- Straight lines or objects may appear wavy and look bent
- Reduced reading vision
Risk Factors
- Age
- Inflammation in the eye (uveitis)
- Severe near-sightedness
- Vitreous traction
- Retinal detachment
- Macula pucker
- Diabetes
- Retinal vein occlusion
- Eye trauma or injury
Treatment/Management



Central Serous Retinopathy (CSR)
Also known as Central Serous Chorioretinopathy, is a sporadic disorder of the outer blood-retinal barrier. It is characterized by a localized detachment of the sensory retina at the macula secondary to focal retinal pigment epithelium (RPE) defects, consequently results in fluid builds up under the retina.
Signs and Symptoms
- Distorted and blurred central vision
- Straight lines may appear wavy or bent in the affected eye (metamorphopsia)
- Micropsia/ macropsia – seeing objects appear in their abnormal size
- Loss of colour saturation
- Diminished contrast sensitivity
Risk Factors
- Emotional stress or type A personality
- Untreated hypertension
- Alcohol use
- Autoimmune disease (ie: systemic lupus erythematosus)
- Organ transplantation
- Gastro-oesophageal reflux
- Cushing’s disease
- Use of steroid (topical, oral, inhaled or through a vein)
Treatment/Management
- Argon laser photocoagulation
- Photodynamic therapy (PDT)
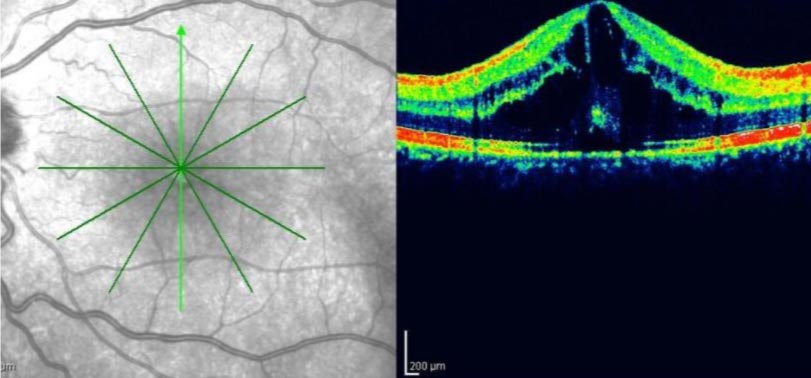
Macular Oedema
It is a condition of the eye that involve accumulation of fluid and swelling of the macula. It occurs due to abnormal leakage and fluid builds up in the macula from damaged or fragile blood vessels in the retina.
Signs and Symptoms
- Reduced central vision
- Distorted and wavy central vision (metamorphopsia)
- Central scotoma
- Difficulty reading and seeing fine details in the affected eye
Risk Factors
- Diabetic retinopathy
- Previous eye surgery (ie: cataract, YAG laser, vitreo-retinal surgery)
- Age-related macular degeneration (ARMD)
- Retinal vascular disease (i.e: diabetic retinopathy, retinal vein occlusion, hypertensive retinopathy)
- Intraocular inflammation (uveitis)
- Retinal dystrophies
- Drug-induced
Treatment/Management
- Anti-VEGF injection
- PRP laser
- Anti-inflammatory treatments
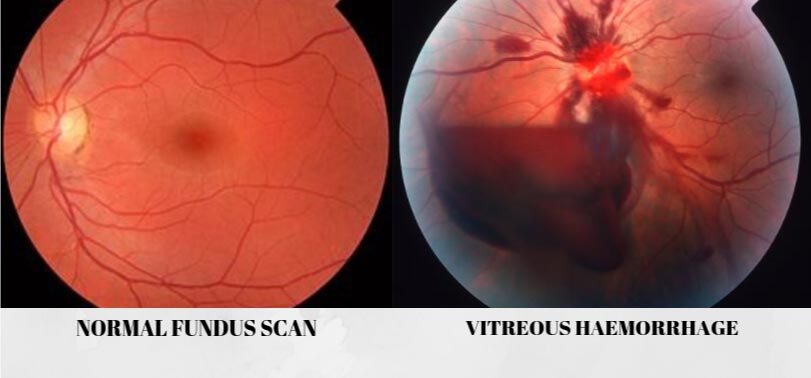
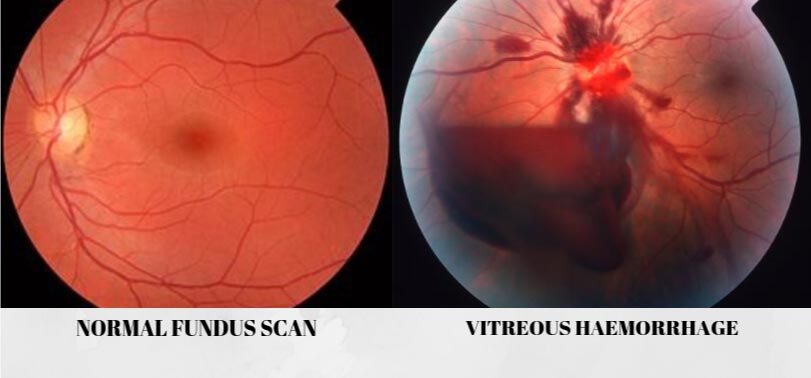
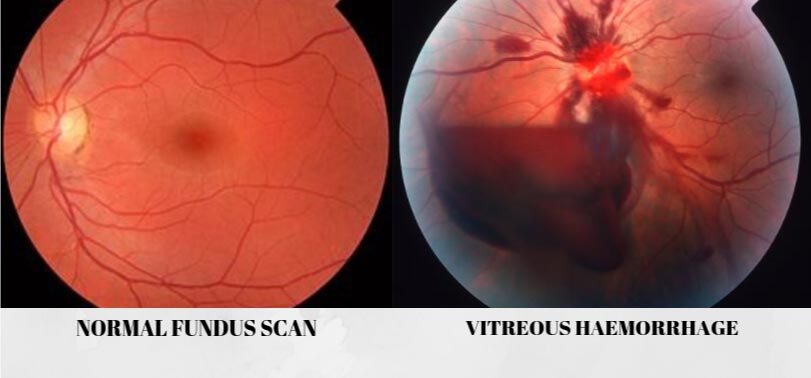
Vitreous Haemorrhage
Bleeding of your vitreous gel inside the eye as a result of numbers of conditions that cause blood to leak from damaged abnormal blood vessels or bleeding from other parts of the eye into the vitreous.
Signs and Symptoms
- Sudden and painless vision loss
- Black spot appearance or floaters on affected eye
Risk Factors
- Damage to normal blood vessels – Ocular trauma or injury can cause normal blood vessel to rupture and lead to bleeding. Eye problems like retinal tear and retinal vein occlusions also can cause damage to normal blood vessels, then lead to vitreous haemorrhage.
- Growth of abnormal blood vessels – new abnormal blood vessels are usually fragile and prone to bleed into the eye, thus cause vitreous haemorrhage.
- Bleeding from other part of the eye – such as from retinal macroaneurysms, tumors and other pathological conditions of the eye that may cause them to bleed into the vitreous.
Treatment/Management
- Scatter pan-retinal photocoagulation (PRP) laser
- Vitreo-retinal surgery – pars plana vitrectomy with endolaser pan-retinal photocoagulation
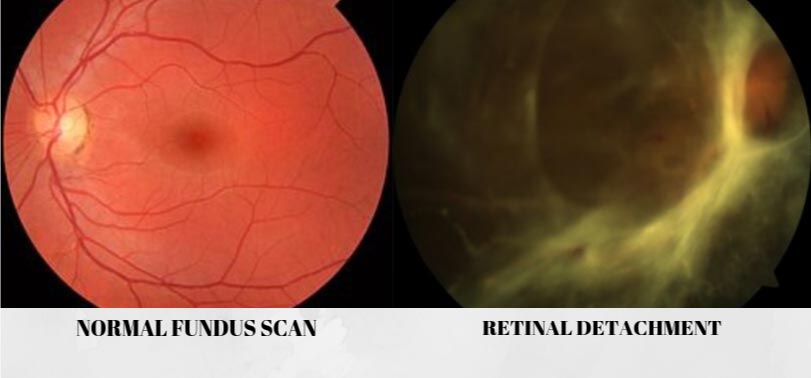
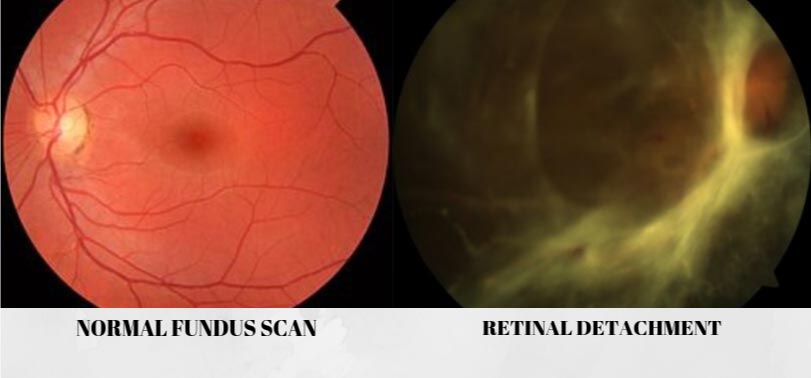
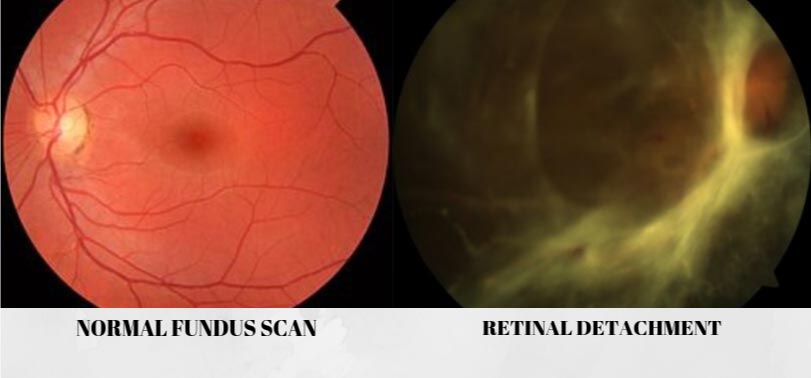
Retinal Detachment
It is an eye condition where the most sensitive layer of the eye which is the retina were separated and peeled away from the back of the eye. Retinal detachment describes the separation of the neurosensory retina (NSR) from the retinal pigment epithelium (RPE) caused by a breakdown of the forces that attach the NSR to the RPE.
This results in the accumulation of subretinal fluid (SRF) in the potential space between the NSR and RPE (Kanski). It is a medical emergency as it is a sight-threatening eye condition.
Signs and Symptoms
- Flashes of light (photopsia)
- Increase in floaters
- Curtain-like visual field defect
- Sudden reduced or loss of vision
Risk Factors
- Aging
- Injury or trauma
- Diabetes
- Extreme near-sightedness
- Previous incidence of retinal detachment in the other eye
- Previous history of major eye surgery (ie: cataract surgery)
- History of other eye diseases (i.e: uveitis)
- Family history of retinal detachment
Treatment/Management
- Vitreo-retinal surgery – vitrectomy where gas/silicone oil is inserted in the eye to help the retina adhere back to the wall of the eye.
- Scleral buckling
Reference:
Kanski Textbook



Ocular Hypertension (OHT)
It is a condition where the pressure inside your eye is elevated higher than 21 mmHg without detectable glaucomatous changes or damages in the eye. The normal intraocular pressure (IOP) range is 11 – 21 mmHg.
Patients with OHT should be monitored closely as they are also known as “glaucoma suspect” and have high risk to get glaucoma.
Glaucoma
It is an eye disease where there is progressive optic nerve damage (neuropathy) characterised by progressive loss of retinal nerve fibre layer, thinning of neuro-retinal rim and irreversible peripheral vision loss. It is usually caused by fluid build ups inside the eye due to various factors and give rise in IOP of more than 21 mmHg.
Common Types of Glaucoma:
-
- Primary open angle glaucoma (POAG) – caused by slow progressive fluid builds up over time due to blocked or clogged eye fluids drainage channels.
- Acute angle closure glaucoma (AACG) – caused by sudden fluid builds up due to blocked or clogged eye fluids drainage channels.
- Secondary glaucoma – caused by other underlying eye conditions such as uveitis (eye inflammation)
Signs and Symptoms
-
-
- Painful red eyes
- Blurred vision
- Peripheral visual field loss
- Haloes around light
- Nausea and vomiting
- Headache
- Sudden vision loss
-
*This condition may even be ASYMPTOMATIC until at the advanced stages!
Risk Factors
-
-
- Elevated intraocular pressure (IOP)
- Older age
- Ethnicity (more common in African, and black individuals)
- Family history
- Short-sightedness (myopia)
- Retinal disease
- Systemic vascular disease (diabetes, hypertension, heart problem)
- Previous ocular trauma, inflammation of the eyes
- Corticosteroid medication (mainly topical)
-
Treatment/Management
-
-
- Medication – course of eye drops
- Laser procedures – trabeculopasty, peripheral iridotomy
- Surgery – minimally invasive glaucoma surgeries (MIGS), trabeculectomy or lens extraction
-
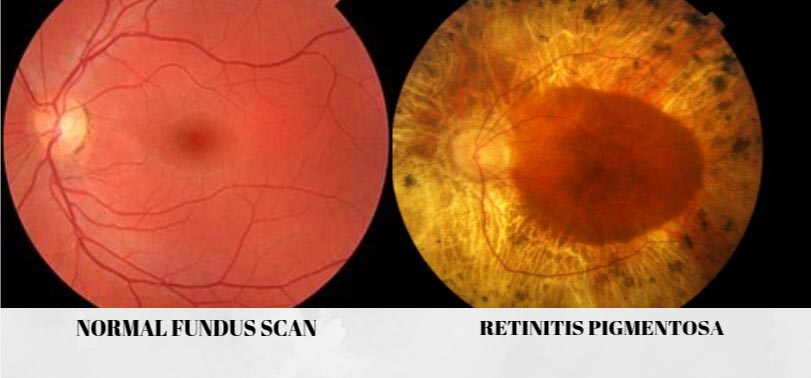
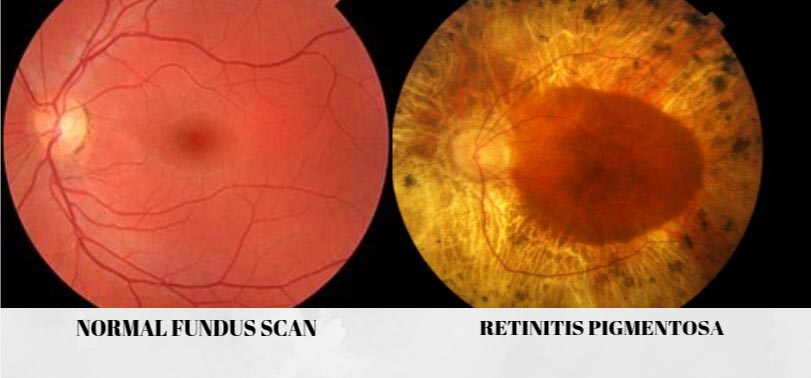
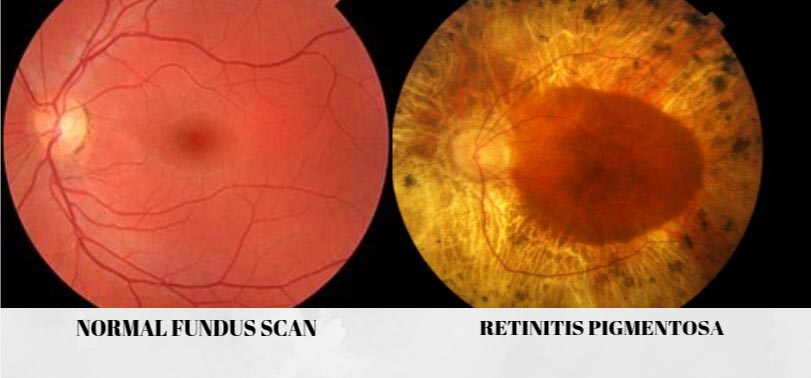
Retinitis Pigmentosa (RP)
RP is an eye disease that causes retinal degeneration. It is a clinically and genetically diverse group of diffuse retinal dystrophies initially predominantly affecting the rod photoreceptor cells with subsequent degeneration of cones (Kanski). Its prevalence is 1:5000. Eventually, people with RP will lose their eyesight.
Signs and Symptoms
-
-
- Difficulty seeing at night (night blindness)
- Gradual loss of vision
- Difficulty doing daily essential tasks such as reading, viewing fine details, driving and recognising faces
-
Treatment/Management
Currently, there are no treatment or cure yet for RP.
However, there are low vision aids and services available to manage and help the patient to cope with the vision loss due to RP.



Floaters
Floaters are faint black or grey entities moving or floating inside the eyes. They are visible or more obvious when looking at clear bright sky or plain blank wall. This condition is usually harmless. However, if it occurs suddenly with increasing numbers of the floaters, seek immediate medical attention, as it may be symptoms of more serious eye condition such as retinal detachment.
Treatment/Management
Usually, most floaters do not require any treatment and are harmless. However, in a serious condition where they affect your vision, there are ways to resolve this:
Book Now
Book Your Appointment
Working Hours:
8:30am – 5:30pm (Monday – Saturday)
Contact Us:
9,10,11, Residensi Park Bukit Jalil, Persiaran Jalil Utama, 57000, Bukit Jalil, Kuala Lumpur